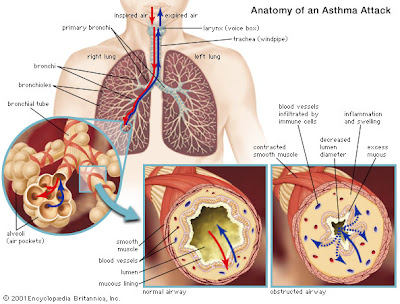
There is no cure for asthma, but the condition can be controlled with various types of drugs. Medications called relievers provide immediate relief for asthma attacks by relaxing (bronchodilation) the walls of the air passages, which widens the passages, allowing air to move freely into and out of the lungs. Long-term treatments called preventers reduce the chronic in- flammation of the lining of the air passages, thereby decreasing the likelihood of an attack and relieving day-to-day discomfort.
Relievers, also known as bronchodilators, are most effective when taken as soon as symptoms of cough- ing, chest tightness, wheezing, or shortness of breath occur. They work within minutes and are effective for four to six hours. The most commonly used bron- chodilators are called beta-2 agonists. As these are inhaled they primarily affect the lungs, which means there are fewer side effects. Another type of medica- tion known as anticholinergics may be given after beta-2 agonists in emergencies to further widen the air passages and reduce mucus production.
Some bronchodilators are long-acting medications that last for at least 12 hours and may be used before exercise or before breathing cold air and to prevent symptoms while sleeping. These longer-acting beta-2 agonists are usually used together with inhaled corticosteroids.
One bronchodilator, theophylline, has been pre- scribed for many years as a long-term control medica- tion for mild to moderate cases of asthma. This is taken daily as a pill, sustained release capsule, or syrup and is particularly effective for reducing symptoms during sleep. Initially it may cause side effects, includ- ing rapid and irregular heartbeats (palpitations), rest- lessness, nervousness, or a headache, but these usually disappear as the body adjusts. To be sure the dose is appropriate, blood levels should be checked periodi- cally. If the level of medication is too low there will be inadequate control of symptoms, while if it is unnec- essarily high, serious heart rhythm irregularities or seizures, as well as nausea and vomiting, abdominal pain, or diarrhea may occur. Aminophylline is a more powerful but pharmacologically similar bronchodilator that is only given intravenously in emergencies.
For long-term treatment of severe chronic asthma, corticosteroids, or preventers, are used. Corticosteroids have long been considered the most effective preven- ter medications because they are anti-inflammatory, and so reduce inflammation in the lining of the air passages. If they are used long-term, however, there is a risk of serious side effects, including cataracts, osteo- porosis (loss of bone mass), and decreased resistance to infection, but as corticosteroids usually are inhaled di- rectly into the air passages, rather than taken internal- ly, these effects are lessened. Nevertheless, inhaled corticosteroids may, sometimes temporarily, affect growth in children.
For individuals with moderate asthma, a group of anti-inflammatory medications called leukotriene modifiers may eliminate the need for cortico- steroids.They are not used for acute attacks but for protection from attacks. These drugs block substances released during an attack that cause more inflamma- tion in the air passages. For more severe asthma, they may be used together with other medications, includ- ing inhaled corticosteroids.
Cromolyn (Nasalcrom) and nedocromil (Tilade) are considered the safest asthma medications currently
available for mild or moderate asthma and are frequently prescribed as preventives for use before exercising. For people with mild or moderate asthma, daily long-term use of these medications may prevent attacks by reducing inflammation in the air passages.
For allergic asthma, allergy desensitization injections (immunotherapy) may decrease sensitivity to allergens in substances such as pollen, insect droppings, or molds. When confronted with an allergen, the body’s immune system manufactures proteins called antibodies. Immunoglobulin E (IgE) is an antibody frequently associated with respiratory allergies. Based on the idea that an allergic attack may not develop if immunoglobulin E is prevented from attaching to cells that release substances which cause allergic asthma, new injectable treatments are under development.